Efficient revenue cycle management (RCM) is an integral part of financial stability for any healthcare center. In this context, athena simplifies medical billing and claim submission through its cloud-based platform, athenaOne.

It includes athenaCollector – a billing and practice management solution designed to automate insurance billing and help healthcare providers get paid faster. This ensures maximum efficiency while reducing the risks of revenue leakage.
This guide outlines the essential steps to submit an insurance bill using athenaCollector while ensuring seamless claim processing.
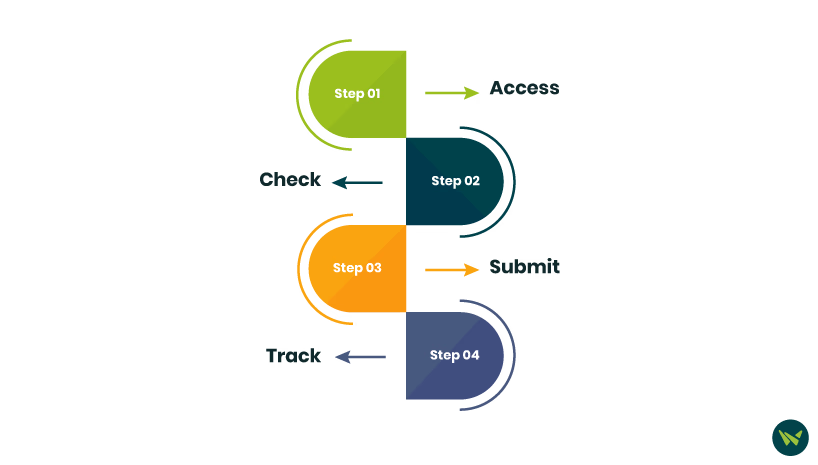
Step 1: Access The Workflow Dashboard
Before the submission of insurance bill, make sure all patient encounters are correctly recorded. Then:
- Navigate to the Workflow Dashboard in athenaCollector
- Identify patient appointments requiring charge entry and confirm that the procedures are documented
- Enter service charges to align with the provider’s documentation for accurate billing
Step 2: Check Claim Accuracy
Athena automatically verifies claim accuracy before submission to prevent errors.
- The claim scrubbing tool scans for coding errors or missing information to accelerate payment cycles
- If flagged, the solution highlights the claims for correction, reducing rejection rates
- Ensure that CPT codes, ICD-10 codes, and modifiers comply with payer-specific requirements

A screenshot of the dashboard of validating Codes
Step 3: Submit The Insurance Claim
Submit the claim for processing once it has been reviewed and scrubbed
- Use athenaCollector for claim management
- Select the verified claim and ensure it is in DROP status (ready to be submitted)
- athena submits batches of claims overnight to insurance payers and clearinghouses

A screenshot of the claim creating on athenaCollector
Step 4: Track Claim Status in athena’s Claims Inbox
- Use the Claims Inbox Tool in athenaCollector to monitor the real-time status of claims
- Athena categorizes the claims based on their current status

A screenshot of Claim status in athenaCollector
Using athenaCollector and its RCM tool can help healthcare providers submit insurance billing, reduce claim denials, and accelerate the workflow. By following the steps mentioned above, practitioners can ensure accurate and timely claim submission while also minimizing financial risks.
For a deeper understanding of athena billing software, check out our detailed blog for tips on using the platform more efficiently.
