Long after the last patient has left and the clinic doors have closed, many healthcare professionals are still glued to their screens. Known as "pajama time," this after-hours work on electronic health records (EHRs) has become a serious concern for clinician well-being, professional retention, and work-life balance.
In a recent survey of 252 U.S. healthcare professionals, we examined the true extent of pajama time, its impact on personal lives, and how certain EHR systems and features are exacerbating or easing the burden.
The boundaries between work and personal life are blurring for healthcare professionals, driven largely by after-hours administrative tasks. This hidden workload is contributing to burnout, strained relationships, and even career reconsideration across the industry.
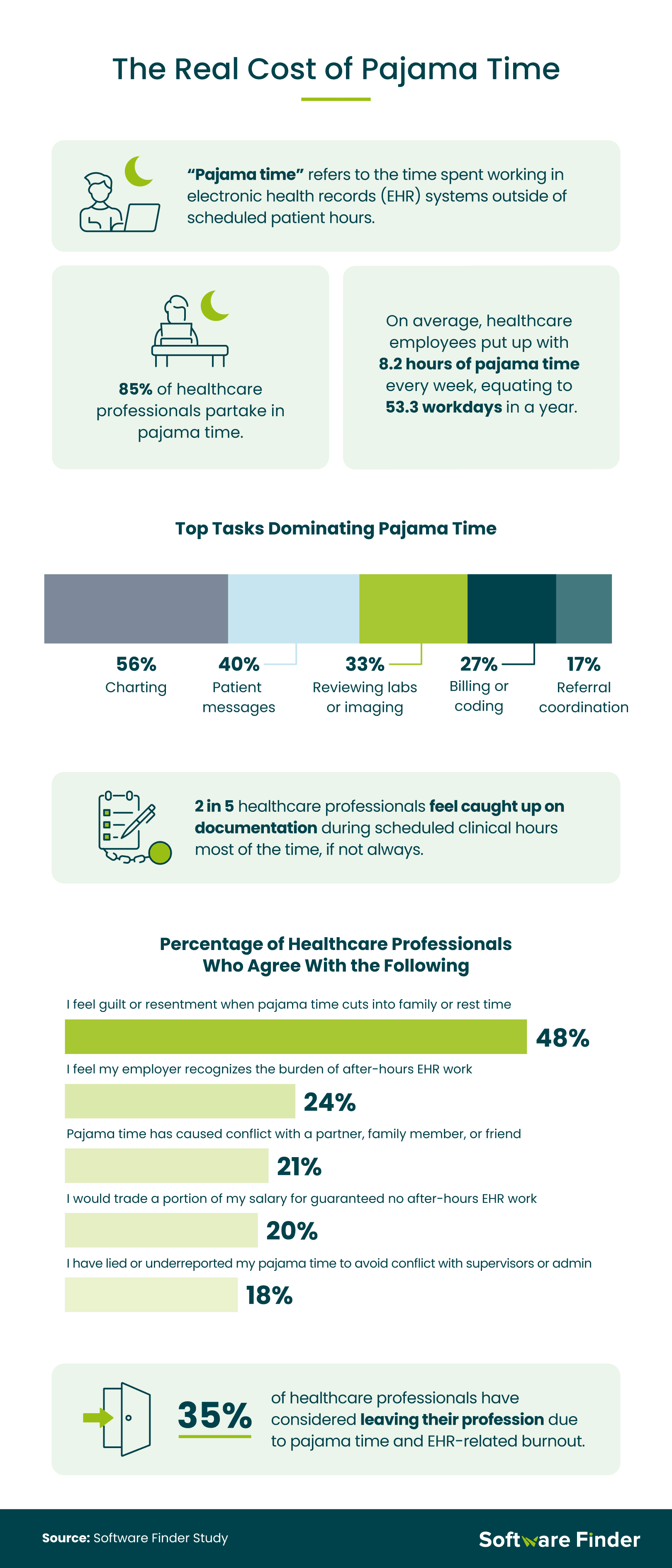
A staggering 85% of surveyed healthcare professionals said they engage in pajama time, with nurse practitioners (NPs) and physician assistants (PAs) leading at 93%. On average, workers logged 8.2 hours of after-hours EHR work each week, which is equivalent to 53.3 full workdays in a year. Outpatient clinic workers reported the highest pajama time at 9.1 hours per week.
Only 40% of healthcare professionals said they always feel caught up on documentation during their regular hours or most of the time. This dropped to 30% among NPs, PAs, and medical technicians, but rose to 48% among registered nurses.
The most time-consuming tasks during pajama time included charting (56%), responding to patient messages (40%), and reviewing labs or imaging (33%). Just 24% felt their employer recognized the burden of pajama time on healthcare workers.
Nearly half (48%) said they feel guilt or resentment when pajama time cuts into family or rest time. Twenty-one percent reported that it has caused conflict with a partner, family member, or friend. One in five clinicians said they would give up part of their salary for a guaranteed promise of no after-hours EHR work. Gen Zers (26%) were more likely to agree with this than Gen Xers (11%).
To avoid workplace tension, 18% of healthcare workers have hidden or underreported their pajama time. Most alarmingly, 35% have considered leaving the profession entirely due to EHR-related burnout, with millennials (37%) being the most likely to feel this way when compared to Gen Z (32%) and Gen X (30%).
The tools clinicians rely on can either ease their burden or make it worse. EHR system design plays a critical role in determining how much time healthcare professionals spend on documentation and how frustrated they feel while doing it.
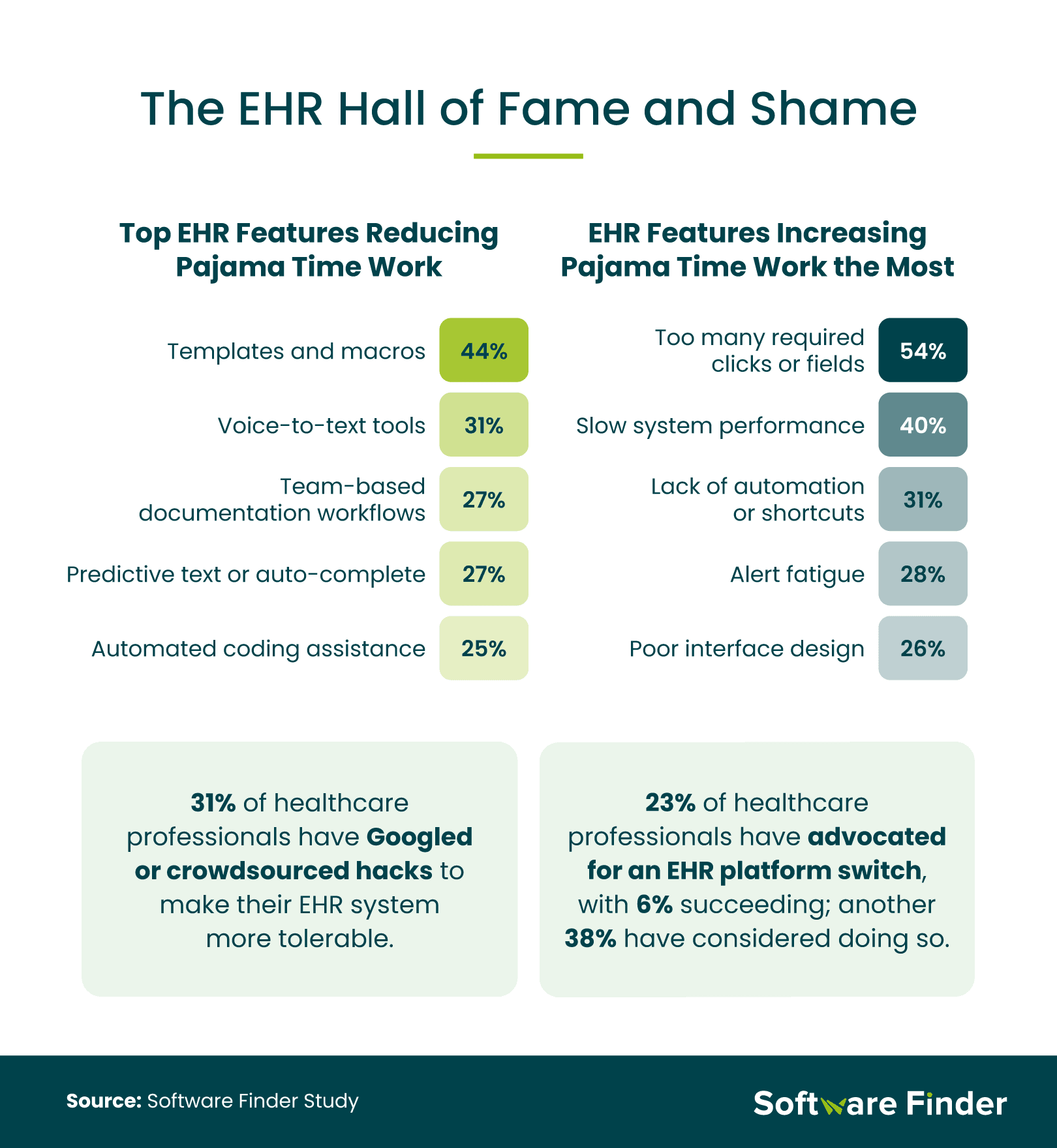
Not all EHR systems are created equal. When asked which features helped reduce pajama time, clinicians pointed to templates and macros (44%), voice-to-text tools (31%), and team-based documentation workflows (27%) as the most beneficial. These features streamline processes and free up valuable hours.
In contrast, EHR designs that require excessive clicks or fields (54%), suffer from slow system performance (40%), or lack automation (31%) were the top contributors to pajama time. The friction these systems create not only extends workdays but also adds to daily frustration.
Some clinicians are taking matters into their own hands. Nearly one-third (31%) said they have searched online for hacks or tips to make their EHR systems more manageable. Physicians were especially proactive, with 59% admitting to this practice. While 23% of healthcare professionals have directly pushed for a change in EHR platforms at work, another 38% have considered doing so.
Beyond lost hours, pajama time is seriously affecting clinicians' well-being. The emotional and mental health impact of after-hours work is affecting how healthcare professionals experience both their jobs and their personal lives.
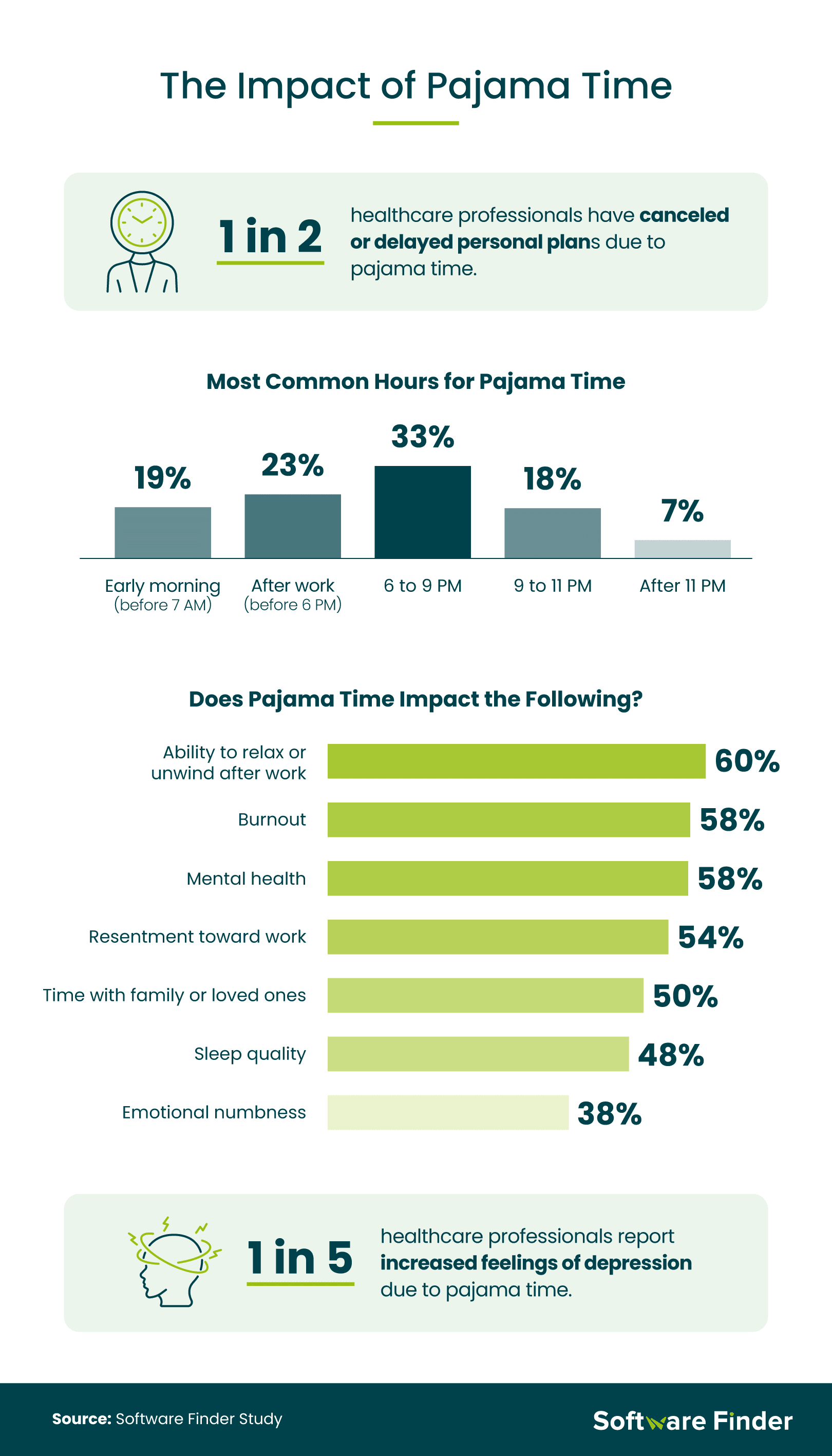
Half of all surveyed healthcare professionals said they've had to cancel or delay personal plans due to pajama time, a number that jumps to 76% among physicians. One in three said their pajama time usually falls between 6 p.m. and 9 p.m., cutting into dinner, family time, or rest.
Burnout is a looming consequence. Eleven percent said pajama time severely impacts their sense of burnout, while 61% said it at least moderately affects their ability to unwind after work. More concerning, 1 in 5 clinicians reported heightened feelings of depression as a result. This emotional strain not only reduces quality of life but also threatens the long-term sustainability of the healthcare workforce.
Pajama time is taking a clear toll on healthcare professionals. It's cutting into their personal lives, adding to daily stress, and making it harder to stay in the profession. Many clinicians are looking for workarounds or even considering career changes because of it. Reducing this after-hours burden starts with better EHR systems and stronger support from healthcare organizations. Giving clinicians the time and space to recharge is essential for their well-being and the future of patient care.
Methodology
For this study, we surveyed 252 healthcare professionals about working on EHR systems outside of work hours, otherwise known as "pajama time." Among respondents, 58% reported as millennials, 20% reported as Gen Z, 17% reported as Gen X, and 5% reported as baby boomers. Additionally, 21% of respondents are registered nurses, 20% are part of a medical office staff, 19% are healthcare administrators, 11% are nurse practitioners or physician assistants, 9% are medical/laboratory technicians, 7% are physicians, and 13% work in a hospital or clinic setting in another role.
About SoftwareFinder
Software Finder helps healthcare providers choose the best EHR software for their needs with expert reviews, tailored comparisons, and personalized consultations. Whether you're a small clinic or a large healthcare system, our platform offers the tools and insights you need to streamline operations and improve clinician satisfaction.
Fair Use Statement
If you'd like to share or report on this study, you're welcome to do so for noncommercial purposes. Just remember to link back to this page and credit Software Finder appropriately.